Why sleep is so important for children with trauma
Dec 2022
Written by Noel Macnamara
Many of you who know me know that I have a big interest in sleep hygiene and the children and young people in out-of-home care (OOHC). To this end, I have put together a small package of material that I hope you will take the time to look at and discuss with your colleagues and carers.
Why is Sleep Important?
As I am sure you know, sleep is an important part of your daily routine. It is estimated that we spend about a third of our time sleeping. Quality sleep – and getting enough of it at the right times – is as essential to survival as food and water.
Sleep is important to several brain functions, including how nerve cells (neurons) communicate with each other. In fact, your brain and body stay remarkably active while you sleep, completing many vital functions, including:
Your brain sorts and processes the day’s information
One of the most active parts of the body during sleep is the brain. There are pronounced changes in the electrical activity of the brain during sleep, which the evidence suggests is a result of the brain’s trillions of nerve cells literally rewiring themselves. This rewiring, which happens during deep, slow-wave sleep, is how we process and are thus able to retain new information we may have learned throughout the day. Your brain is making a map of the information, making new connections, and breaking other ones.
Hormones flood your body
There are various hormones released during sleep, all with different purposes. Melatonin, released by the pineal gland, controls your sleep patterns. Levels increase at night-time, making you feel sleepy. While you’re sleeping, your pituitary gland releases growth hormone, which helps your body to grow and repair itself.
Your sympathetic nervous system chills out
During sleep, the sympathetic nervous system – which controls the fight or flight response – gets a chance to relax. Studies have shown that when we’re deprived of sleep, sympathetic nervous system activity increases, which is also mirrored by an increase in blood pressure. There are a number of studies investigating whether there’s a relationship between decreased sleep duration and increased risk of heart disease (Castro-Diehl et al., 2016).
Cortisol levels lower
Levels of cortisol, often called the stress hormone, decreases during the first few hours of sleep before rising to peak soon after you wake up. This helps makes you feel perky when you wake up and switches on your appetite.
Your muscles paralyse
During REM sleep – the deep sleep where most recalled dreams occur – your eyes continue to move but the rest of the body’s muscles are stopped, potentially to prevent injury.
During this stage, your muscles are temporarily paralysed, meaning you can’t move. Some scientists think this might be so that you don’t physically act out your dreams (Brooks & Peever, 2012).
Anti-Diuretic Hormone (ADH)
Vasopressin, or ADH is an anti-diuretic hormone released by the brain under a circadian rhythm that switches off the need to urinate so often overnight. When you sleep, your body increases its production of ADH, signalling your kidneys to keep absorbing and recycling water, preventing the creation of urine. Some water still passes through to the bladder, slowly filling it up. This, along with the suppression of ADH as you wake up, is why most people have to urinate first thing in the morning.
Your immune system releases inflammation-fighting cytokines
Sleep and the circadian system exert a strong regulatory influence on immune functions (Besedovsky, Lange, & Born, 2012). While you’re sleeping, your immune system releases a type of small proteins called cytokines. If you’re sick or injured, these cytokines help your body fight inflammation, infection, and trauma. Without enough sleep, your immune system might not be able to function at its best.
Recent findings suggest that sleep also plays a housekeeping role that removes toxins in your brain that build up while you are awake.
Evidence shows that sleep affects almost every type of tissue and system in the body and that a chronic lack of sleep can increase the risk for non-communicable diseases such as high blood pressure, cardiovascular disease, diabetes, depression, and obesity.
If you would like to know more about sleep, watch this short video:
How does trauma affect sleep?
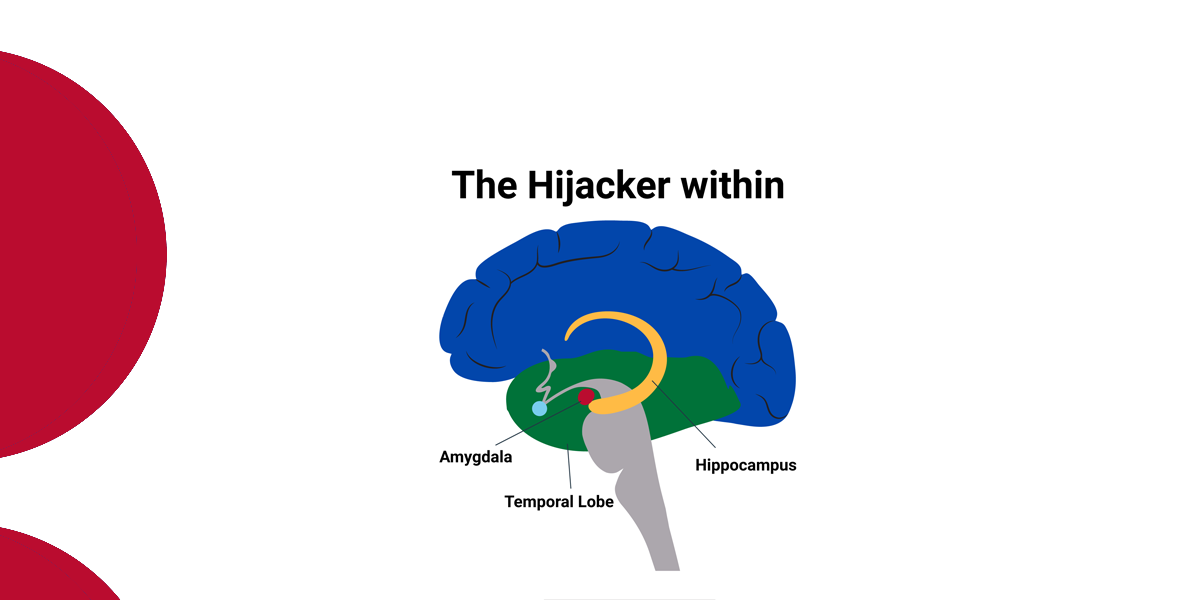
Traumatic experiences can negatively affect the quality and amount of sleep that a child or young person gets. Both physical and sexual abuse can significantly disturb sleep (Glod et al., 2006). The brain can be overstimulated after trauma and may experience an influx of adrenaline. That, coupled with being extremely or excessively aware (hyper-arousal or hyper-awareness), may make it difficult to fall and stay asleep.
Children who experience flashbacks, may experience them just as frequently at night as they do during the day. They may also experience nightmares, which can startle them awake and make falling back asleep extremely difficult. A child or young person’s environment may also affect sleep – for example, a dark room may create a higher level of anxiety, or complete silence may make someone more nervous about sounds that would ordinarily not be noticeable.
Sleep, Mental Illness and Substance Misuse
Symptoms of mental illness and substance misuse are common features of young people in OOHC. The link between poor sleep quality, delayed sleep timings, and irregular sleep-wake cycles and mental ill-health is not new. (See: Castro et al., 2015; Lunsford-Avery et al., 2017.) Sleep problems are commonly listed as core symptoms of many psychiatric disorders, including major depressive disorder (MDD) and generalised anxiety disorder (GAD). However, we are now able to recognise that sleep problems may also be a causal factor in the development of such psychiatric disorders. This bidirectional perspective is in sharp contrast to the previously often held belief that sleep problems were secondary to a psychiatric disorder, and thus rarely diagnosed or targeted in mental health care interventions.
In a recent article, Shetty et al. (2020) investigated the link between sleep disturbance, chronotype – chronotype is the natural inclination of your body to sleep at a certain time, or what most people understand as being an early bird versus a night owl – and psychotic symptoms.
The results showed that young people who were at ultra-high risk of developing psychosis and who were ‘night owls’, had higher negative psychotic symptoms. Dr Hartmann described negative psychotic symptoms as including: “not showing emotions, being withdrawn and showing a lack of social interaction and motivation”. She also added, “These symptoms are notoriously difficult to treat”.
Shetty et al. (2020) also found that there is emerging evidence that we can change a person’s chronotype, so we can try to intervene to shift someone who is a night owl to an earlier period of the day over time, this could also impact on negative psychotic symptoms.
Substance Misuse
The association between substance use and sleep problems appears to be bidirectional, with sleep problems increasing risk for developing substance use disorders, and acute and chronic substance use leading to acute and chronic problems with sleep (Haario, Rahkonen, Laaksonen, Lahelma, & Lallukka, 2013).
Overwhelming evidence points to chronic alterations in sleep from chronic use of addictive substances that may be distinct from some or all of the acute effects of those substances. Interestingly, the effects of chronic use on sleep are similar among both central nervous system stimulants and depressants.
Decreased sleep time, increased sleep latency and wake time after sleep onset, and deficiency in slow-wave sleep generation appear to be common to chronic use of alcohol, cocaine, cannabis, and opiates. REM sleep is also affected by acute and chronic use but may be more sensitive to the pattern or quantity of recent use and time from last use, as results vary more among studies.

Conclusion
Identifying sleep problems in children and young people can help prevent the onset and worsening of mental illness, substance misuse, and other health impairments. Thus, identifying a child or young person’s sleep pattern as a part of any assessment can be extremely important to enable appropriate forms of intervention to take place. This can be as simple as helping the child or young person to re-orient their day towards being an early bird rather than a night owl. It may require other forms of intervention such as melatonin.
Melatonin is a natural hormone that is produced by the pineal gland in the brain and then released into the bloodstream. Darkness prompts the pineal gland to start producing melatonin while light causes that production to stop. As a result, melatonin helps regulate circadian rhythm and synchronise our sleep-wake cycle with night and day. In doing so, it facilitates a transition to sleep and promotes consistent, quality rest.
Studies have found that melatonin can improve sleep in certain cases, but it isn’t for everyone. It is important to be aware of and carefully consider melatonin’s potential benefits and downsides.
Sleep is a complex and dynamic process that affects how you function in ways that we are now beginning to understand. Put simply, sleep is vital to good physical and mental health!
Resources
Sleep and young people – Myth Busting about Sleep
References
Besedovsky, L., Lange, T., & Born, J. (2012). Sleep and immune function. Pflugers Archiv European Journal of Physiology, 463(1), 121–137. https://doi.org/10.1007/s00424-011-1044-0
Brooks, P. L., & Peever, J. H. (2012). Identification of the transmitter and receptor mechanisms responsible for REM sleep paralysis. Journal of Neuroscience, 32(29), 9785–9795. https://doi.org/10.1523/JNEUROSCI.0482-12.2012
Castro-Diehl, C., Diez Roux, A. v., Redline, S., Seeman, T., McKinley, P., Sloan, R., & Shea, S. (2016). Sleep duration and quality in relation to autonomic nervous system measures: The multi-ethnic study of atherosclerosis (MESA). Sleep, 39(11), 1927–1940. https://doi.org/10.5665/sleep.6218
Glod, C. A., Teicher, M. H., Hartman, C. R., & Harakal, T. (1997). Increased nocturnal activity and impaired sleep maintenance in abused children. Journal of the American Academy of Child and Adolescent Psychiatry, 36(9), 1236–1243. https://doi.org/10.1097/00004583-199709000-00016
Haario, P., Rahkonen, O., Laaksonen, M., Lahelma, E., & Lallukka, T. (2013). Bidirectional associations between insomnia symptoms and unhealthy behaviours. Journal of Sleep Research, 22(1), 89–95. https://doi.org/10.1111/j.1365-2869.2012.01043.x
Shetty, J. J., Nicholas, C., Nelson, B., McGorry, P. D., Lavoie, S., Markulev, C., Schäfer, M. R., Thompson, A., Yuen, H. P., Yung, A. R., Nieman, D. H., de Haan, L., Amminger, G. P., & Hartmann, J. A. (2021). Greater preference for eveningness is associated with negative symptoms in an ultra-high risk for psychosis sample. Early Intervention in Psychiatry, 15(6), 1793–1798. https://doi.org/10.1111/eip.13112

![CETC [Why sleep is so important for children with trauma]-blog--feature-image](https://www.cetc.org.au/wp-content/uploads/2022/12/CETC-Why-sleep-is-so-important-for-children-with-trauma-blog-feature-image.png)